 Life Is What You Make It
Life Is What You Make It
Len Strickland
I am Len Strickland and I was diagnosed with Hereditary Amyloidosis (ATTR) with a variant of Val122ile. There are over 100 different variants of ATTR based on culture and ethnicity. I learned of my affliction at the Mayo Clinic in Rochester, Minnesota on March 29 of 2007.
Hereditary Amyloidosis (ATTR and non-TTR) is a rare type of Amyloidosis that is caused by an abnormal (mutant) gene. Several abnormal or mutant genes can cause hereditary amyloidosis. There are other systemic types as well: AL, AA, and Wild-Type ATTR.
My symptoms began in August of 2006. They included dizziness, shortness of breath after exercising (aerobics and power walking), extreme tiredness after walking up a flight of stairs, heart palpitations and edema in my ankles, feet and calves. I consulted my primary care physician and was given an EKG that showed a slight abnormal blip. He referred me to the in-house cardiologist who gave me an echocardiogram and put me on the treadmill. The cardiologist noticed an enlargement in my right ventricle and thickened heart walls. I was treated for congestive heart failure, but it was felt that a consultation was necessary from colleagues at Stanford University and the Mayo Clinic in Scottsdale, Arizona.
Both Cardiology Departments at Stanford University and the Mayo Clinic indicated symptoms of Amyloidosis, but without further tests they could not be sure of what type. After that I had a heart biopsy, heart catheterization and numerous blood tests. My cardiologist referred me to the Mayo Clinic in Rochester, MN.
Fast forward to March 4, 2008, when I was officially placed on the regional heart transplant list (a radius of 1500 miles). The categories of placement are 1A, 1B and 2 with 1A being the most severe and the top of the list. I was a 2 and told to keep my hopes at a minimum.
The only good news was that my blood type is AB positive, which means I was a universal recipient and could receive all donor hearts with “positive” (+) blood types. At the time, I was the only AB+ blood type on the list, therefore, my chances of receiving a new heart due to blood type was the only positive news.
On Tuesday evening June 10th, at a little after 10 pm, I received a call from UCSF’s Chief Cardiac Surgeon notifying me that they had a match for my new heart. Shortly after 1:45 am, Wednesday morning, my wife, Karen, and I arrived at UCSF. I was admitted for surgery immediately. I went into surgery shortly after 11 am on Wednesday, June 11th. It was 11½ hours later that I had a new heart. My donor was a 23 year-old male; he would have been 30 years old on September 17, 2014. Three months and 1 week after placement on the bottom of the list, I had a new heart.
What is astounding is that the heart was a perfect match. I cannot stress enough the enormity of the care I received by the UCSF doctors and medical staff during my recovery. Receiving a new heart is one thing, but the care was enormous. The UCSF Medical Center released me on Friday, June 20th. I felt great; however, I still had a long way to go before full recovery and adjustment to all of the immuno-suppressants and other medications.
Fortunately, I have had excellent health insurance. With the exception of deductibles and co-pays for medications, most of my health concerns were, and are, covered. However, all other expenses, such as lodging, transportation, food, co-pays and deductibles were not covered; costs did add up and were all out-of-pocket. What was above and beyond anything I would have ever expected was that, on March 11, 2008, friends, Rotarians and business associates of mine had a fundraising dinner in my honor and raised $15,000 for our out-of-pocket expenses.
The money really came in handy to pay for all of our out-of-pocket expenses as mentioned above. Post-transplant care and recovery required that Karen and I stay at a Hotel in San Francisco close to UCSF for treatment on an on-going basis until the doctors and the rest of the heart transplant team felt comfortable with my progress.
The recommended length of stay is generally 30 to 45 days, but it can vary, based on a patient’s progress. The first 6 months are the most critical, but overall I had health and activity restrictions for one year post-surgery. I am extremely fortunate and blessed for my new heart as the ultimate “gift of life” that has given me a new lease on life. Arguably, the most stimulating aspect of this journey is that Karen and I can now look forward to things we used to do together prior to this disease.
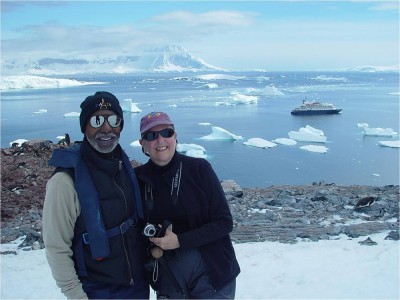
Not only am I able to spend time with my wife, I am able to spend quality time with my grandchildren. We are extremely fortunate and blessed to have been able to travel, live our lives as we do and see for ourselves the world as we have often read in books, magazines and watched on TV.
We are continuing to resume our lives and travels as if nothing ever happened. I will continue to tell my story to encourage others. If I can do it through positive thoughts and determination, you can as well. Life is what you make it!
